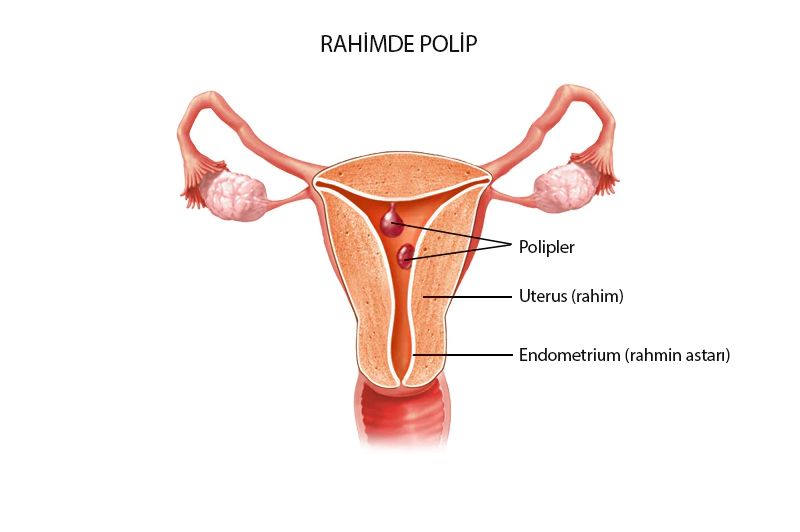
Endometrial Polyp
The tissue that lays inside the uterus and which we throw out every month is also home to our pregnancies. This area is called endometrium tissue.
Endometrial polyps are benign formations that result from endometrial tissue, and the endometrium tissue is enlarged in some areas and pushed towards the intrauterine tissue. It is formed by excessive thickening of the intrauterine tissue surrounding a central vein. This cambered area can fit into the intrauterine tissue with a wide base, but it often clings with a handle. There may be one or several. The formation in the form of a piece of meat, also called a polyp, can take place in the cervix, which will then be called a cervical polyp. The sizes of endometrial polyps can range from 1 to several centimetres.
Frequency of Endometrial Polyps
The frequency is higher before menopause, and 60% of its polyps are women before menopause. It is extremely rare before puberty. It is mostly observed after the age of 40. In the pathological examination of women who underwent hysterectomy, endometrial polyp was detected between 10-25%, regardless of whether they cause symptoms or symptoms.
Risk Factors of Endometrial Polyps
The role of estrogen in the formation of endometrial polyps is indisputable. When the risk factors are examined, this will be clearly understood.
These risk factors are:
advanced age
late menopause
never gave birth
obesity
hypertension
diabetes
Tamoxifen use in breast cancer maintenance treatment
It can be listed as estrogen replacement therapy in menopause.
The Relationship of Endometrial Polyps With cancer
Although there are contradictory opinions about the cancer potential of endometrial polyps, the majority are benign structures and do not contain significant cancer potential. However, endometrial polyps in menopause should be removed and cancer should be excluded.
Findings of Endometrial Polyps
In women who have no complaints in the clinic, it is quite common to be caught by ultrasonography. It appears as a symptom and with frequent bleeding. These bleeding can be in the form of increased menstrual amount, spotting before and after menstruation, prolonged menstrual period or interim bleeding at unrelated times. Bleeding is also the main symptom after menopause. They are slightly more likely to give symptoms after menopause.
Cramp-like pains may occur when the nutrition of the tissue in the polyp is disturbed or the large polyp is born into the vagina.
In cases where the polyp occupies the endometrium and is close to the entrance to the tub, it can lead to inability to conceive or to recurrent pregnancy loss.
Diagnosis in Endometrial Polyps
Ultrasonography is very useful in diagnosis and it can be easily seen as a hyperechogenic area within the endometrial tissue, especially when performed at the end of menstruation. Histerosonography is a frequently used method to confirm the diagnosis. With the help of a cannula, saline solution is given to the endometrial tissue, while vaginal ultrasonography is monitored as endometrial polyp hyperechogenic, stalk or broad-based. An important advantage of sonohysterography is that the localization of polyps in the uterus can be determined.
Medicated uterine film called hysterosalpingography can also be observed as filling defect in the intrauterine tissue. It should not be forgotten that it is not necessary to take every polyp in the treatment. There is no need to remove polyps before menopause and less than 1 cm. It will be sufficient to monitor the woman at certain intervals depending on her condition.
Treatment in Endometrial Polyps
If the polyp causes complaints, if it is over 1 cm or if the woman is after menopause, it will be useful to take the polyp. Regardless of the size, if microinjection will be applied, it is a better option to take polyp beforehand.
The gold standard in surgical treatment is hysteroscopical polypectomy. Office hysteroscopy can be performed in office conditions without anaesthesia without the need for an operating room. However, it is more preferred to apply it in operating room conditions under general anaesthesia. The advantage of hysteroscopy to abortion is that the location of the polyp is clearly visible and the polyp root can be completely removed. In this way, the possibility of recurrent endometrial polyp after abortion can be eliminated. The procedure usually takes quite short time and the probability of water poisoning, which is the biggest complication of hysteroscopy, is very low. However, puncture of the uterus, bleeding or infection may be in abortion, or in hysteroscopy. Hysteroscopy can be easily applied in case of bleeding in menopause. The possibility of cancer is not a contraindication to hysteroscopy.
During the abortion, the surface of the polyp may be slippery, so it cannot be removed and can be partially removed without the polyp root. At the same time, early diagnosis of cancer can be missed in postmenopausal women. Therefore, it would be appropriate to apply hysteroscopy whenever possible.






 Turkish
Turkish Deutsch
Deutsch Bu İçeriği Beğendim
Bu İçeriği Beğendim