Congenital Abnormalities of Uterus
Female and male embryos in the womb have two pairs of genital ducts. While mesonefric channels (Wolff channels) play an important role in the development of the male reproductive system, paramezonefric channels (Müller channels) provide female reproductive system development. As a result of the abnormal development of the Mullerian ducts, as a result of the inability of the genital organs to fully merge into the midline, if Uterus didelfis, partial merging problem: Uterus bicornus, with incomplete absorption of Müller ducts, Uterin Septum, if there is a problem in the development of a Müller duct: Uterus unicornia, and rarely Mullerian agenesis is observed.
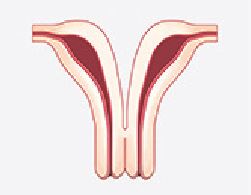
Uterus didelfis occurs as a result of the merging of the Mullerian Channels to the midline. It contains two uterine corners, two cervical cavities and a horizontal (longitudinal) vaginal septum. It does not give symptoms in many patients. In general, the diagnosis is made by noticing the longitudinal vaginal septum and double cervix (cervix) during routine examination. If any of the vagina cannot be opened out, the blood coming from the menstrual accumulates and hematocolpos is formed. Therefore, diagnosis can be made while investigating the developing pelvic pain. In the presence of one of the two vagina closed (if it cannot be opened out), the same-sided renal agenesis (absence of kidney) is usually observed. Uterus didelfis can cause preterm labour, spontaneous and recurrent miscarriage, fetal development and arrival anomalies (breech arrival, lateral posture). Treatment depends on diagnosis and present. In the presence of unilateral vagina with obstruction and pain in sexual intercourse, the vaginal septum is removed. The positive effect of surgical treatment on pregnancy results has not been shown.
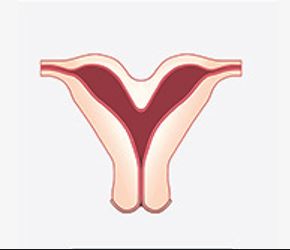
Uterus Bikornus: It results from an incomplete junction of the bilateral Müller channel at the fundus level. After the arcuate uterus, Mülleryan forms the major part of channel fusion anomalies. It has little effect on reproduction and poor pregnancy outcomes. Pregnancy complications are repetitive. Although there are cases such as recurrent miscarriage, preterm birth, anomaly of the fetus, rest of the placenta in the womb (rest placenta), the subsequent pregnancy is often better. In differential diagnosis, HSG of the uterine septum with the bicornus uterus is insufficient. Therefore, definitive diagnosis is made in direct observation with laparoscopy. The treatment is surgical and it can be considered in patients with recurrent pregnancy loss after other causes are excluded. Strassman surgery in the bicornus uterus was performed more frequently in the old years to create a sufficient intrauterine east, but it is a decision that the pregnancy success may not be as desired and a more risky pregnancy will occur due to the large incision made.

In uterus unicornia anomaly, the uterus developed from unilateral Müller channel. On the opposite side, a rudimentary horn with a functional endometrium may be associated with the unicornus uterus. If there is no connection with the rudimentary horn containing functional endometrium, hematometra may develop. In this case, the patient presents with pelvic mass and pain. If there is a connection with rudiment horn, the patient is at risk for rudimentary cornual pregnancy. The treatment is appropriate to be removed surgically depending on the presence of rudiment horn and whether this horn is functional or not.

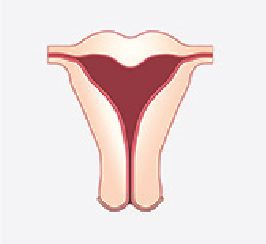
Uterine septum is the most common anomaly among the Mullerian canal anomalies. Spontaneous abortion causes repeated pregnancy losses and preterm labour. Patients with a recurrent miscarriage should be evaluated for uterine septum. However, other recurrent miscarriages must be ruled out before attaching it to the septum. The most accurate way to separate the uterine septum from the bicornus uterus is laparoscopy. In the presence of the septum, a notch is observed in the middle while the fundus is in normal view. At this point, it is a method we can easily use in the clinic to make a differential diagnosis between the three-dimensional USG, which we use very professionally, and the uterine septum and the uterine septum. Its treatment is to cut the septum and open the intrauterine tissue surgically by hysteroscopy.
Uterus Arcuatus is a minor anomaly of the uterus. Myometrium in the fundus makes a slight indentation towards the cavity. Those who consider it a variant of normal are common. While 33.6% of congenital uterine anomalies were uterine septum, the arcuate uterus was found to be 32.8%. There was no decrease in fertility and increased risk of pregnancy-related complications. However, in cases of recurrent IVF failures and recurrent miscarriages, if intrauterine tissue is also accompanied by T-shaped intrauterine tissue, intrauterine tissue can be expanded to some extent.
The embryological migration of the uterus and the migration of the ovaries and the tubes are not unique, so the ovaries are monitored in uterine anomalies. Tubes can be affected at the point of entry into the uterus according to the severity of the junction anomaly. In the meantime, kidney and urinary tract anomalies can be frequently encountered in the uterus’s congenital abnormalities and must be evaluated in detail.
Cervical insufficiency appears to be more common. Sometimes these problems can be diagnosed with ultrasound by examination or uterine films. It is generally diagnosed with painless opening of the cervix and preterm delivery in the period of 12-28 weeks, which is called the second trimester of pregnancy. If the diagnosis is confirmed and early opening of the cervix and premature birth cannot be associated with another reason, stitches can be placed in the cervix at the end of the first trimester during subsequent pregnancies.






 Turkish
Turkish Deutsch
Deutsch Bu İçeriği Beğendim
Bu İçeriği Beğendim