Extrauterine Pregnancy Development (Ectopic Pregnancy)
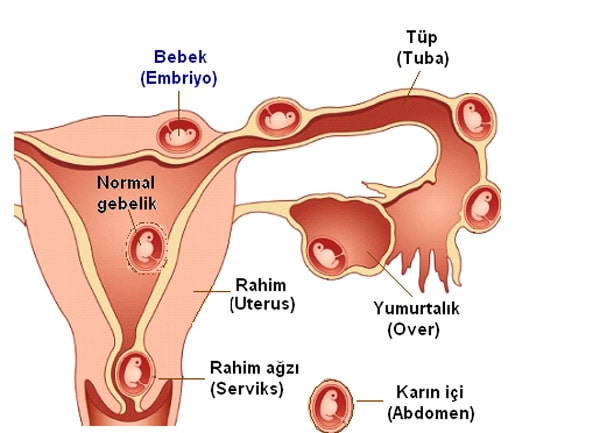
It is the placement of the fertilized ovum (pregnancy material), which is formed as a result of the merger of the sperm and the egg, in any part of the genital canal or in the pelvis, except for the usual localization of the uterine cavity. It is most often located in the fallopian tubes (tubal pregnancy). Apart from this, it can be in the ovary, cervix, between the ligaments of the uterus (intraligamentary) or at the same time both inside and outside (heterotopic pregnancy).
Frequency of Ectopic Pregnancy
Its frequency has increased four times in recent years. In addition to the fact that more accurate diagnosis is made with the increase of diagnostic possibilities, pelvic infection, late delivery and assisted reproductive techniques seem to be effective. Today, ectopic pregnancy rates are around 1-2%.
Despite the development in early diagnosis and treatment methods, ectopic pregnancy still maintains high risk rates in terms of maternal deaths and complications after ectopic pregnancy. External pregnancies are responsible for approximately 10% of pregnancy-related maternal deaths. Here, the risk of late detection or misdiagnosis of the case by the woman or physician increases the risk. Today, developing hormone laboratory technology and the use of high technology ultrasonography provide confidence in terms of early diagnosis, and many different diseases in the abdomen and pelvis make the differential diagnosis difficult.
Risk Factors for of Ectopic Pregnancy
* As the female age increases, the risk of ectopic pregnancy increases. The risk increases 3-4 times between the ages of 15-24 and 35-44.
* Previous pelvic infections increase the risk of ectopic pregnancy both by impairing the movement of the tubes with adhesions and damaging the tissue inside the tube. As the number of previous pelvic infections increases, the likelihood of ectopic pregnancy increases. Chlamidia, ureoplasma, anaerobic bacteria and gonorrhoea can be the cause of infection. While partial narrowing decreases the mobility of the tube, if both tubes are completely blocked, pregnancy will not be possible.
* Assisted reproductive techniques increase the risk of ectopic pregnancy. Ovulation (obtaining a large number of eggs after ovulation induction and increasing the number of embryos may increase the risk, as well as pathologies that affect the movement of the tubes, such as previous pelvic infection or endometriosis, which may be the cause of infertility.
* Having an ectopic pregnancy before will increase the likelihood of ectopic pregnancy to 10% in the next pregnancy.
* Opinions about the risk of ectopic pregnancy when using intrauterine devices are contradictory. There are also opinions suggesting that it decreases in addition to the views that find a little more risky in terms of ectopic pregnancy, especially because intrauterine devices containing progesterone hormone decreases tube movement with the effect of progesterone. In intrauterine use, the risk of ectopic pregnancy seems to be more related to the presence of infection.
* 30-40% of pregnancies occurring after tube ligation will be followed by ectopic pregnancy. It is known that the risk of ectopic pregnancy increases when pregnancy occurs in unsuccessful use of prevention methods.
* In women who previously had intra-abdominal operations (ovary cyst, appendectomy, fibroid surgery, etc.), the tubes may be affected due to adhesions that may be seen after the operation in the abdomen and the possibility of an ectopic pregnancy increases. Microsurgery operations related to previously passed tubes also significantly increase the risk.
* Women who smoke more than a pack of cigarettes a day are more likely to experience ectopic pregnancy because they reduce the movement of nicotine tubes.
* Although rare, congenital deformities in the tubes may cause ectopic pregnancy.
Locations of Ectopic Pregnancy
95% of ectopic pregnancy occurs in tubes. Less likely, it can occur in the localization, where the uterus, called the cornu region, joins the tubes, in the cervix, ovaries, on the old caesarean section and in the abdominal cavity.
Signs/Symptoms of Ectopic Pregnancy
All symptoms seen in the early period of a normal pregnancy may also occur in ectopic pregnancy. There may be a positive pregnancy test in the blood or urine, menstrual delay, nausea. In addition, pain of varying severity, abnormal vaginal bleeding, shoulder pain or fainting may occur in the lower abdomen. When the feeling of faintness was seen, the external pregnancy product could not expand the tube any more, the tube was torn and intra-abdominal bleeding. At this point, life risks started. The important thing is that both the patient and the doctor suspect the diagnosis before reaching this point.
In cases of abnormal vaginal bleeding with menstrual delay, it is necessary to contact the physician as soon as possible.
Diagnosis in Ectopic Pregnancy
Regardless of the above signs, all symptoms seen in the early period of a normal pregnancy may also occur in ectopic pregnancy. There may be a positive pregnancy test in the blood or urine, menstrual delay, nausea. In addition, pain of varying severity, abnormal vaginal bleeding, shoulder pain or fainting may occur in the lower abdomen. When the feeling of faintness was seen, the external pregnancy product could not expand the tube anymore and the tube was torn and intra-abdominal bleeding develops. At this point, life risks started. The important thing is that both the patient and the doctor suspect the diagnosis before reaching this point.
In cases of abnormal vaginal bleeding with menstrual delay, it is necessary to contact the physician as soon as possible.
Although the pregnancy test is positive, the inability to see the gestational sac in the intrauterine tissue will be the first step to suspect.
With transvaginal ultrasonography, the mass containing the gestational sac can be detected in the tube. While it can be monitored in the gestational sac found in the tube, it is not possible to see the mass containing the gestational sac from time to time. In intraabdominal bleeding, a varying amount of free and clotted blood can be observed.
The rate of increase in β-HCG values is very helpful in diagnosis. It is often characterized by an inadequate increase. In a normal pregnancy, an increase of 66% and more is sought in HCG values, which are examined at 48-hour intervals. In case of insufficient increase, the decision should be revised. Especially in HCG values exceeding 1500, it is absolutely necessary to see the gestational sac in the intrauterine area. If not, the probability of an ectopic pregnancy diagnosis will increase.
In the differential diagnosis; early normal pregnancy, threats of miscarriage and incomplete abortions, acute pelvic infection, appendicitis, fibroid degeneration, ovarian cyst rupture and ovarian cyst torsions should be kept in mind.
Very rarely, normal pregnancy in the uterus can be combined with an ectopic pregnancy and it is called “heterotopic pregnancy”. Its frequency has been reported as 1/30000.
Treatment of Ectopic Pregnancy
Holding/Waiting Treatment
In general, up to 18% of ectopic pregnancies are spontaneously resorbed and do not require any treatment. If we are diagnosed during the process of resorption and we can watch the mass regress with the decrease of HCG and if there is no intra-abdominal bleeding, close follow-up can be performed. It can be a choice in cases where the HCG value is below 1000. It must be ensured that the external pregnancy is in the tube, the mass is below 4 cm and there is no intra-abdominal bleeding. The patient must be hospitalized. In selected treatments, waiting treatments were successful in 70% of patients. Follow-up without any treatment is generally a difficult choice for administration. If the process does not go as expected, the tube may rupture with increased pressure and intra-abdominal bleeding may occur. In this case, tube loss will have occurred.
Medical Treatment
The most widely used agent in medical therapy is methotrexate. If there is no intra-abdominal bleeding and ectopic pregnancy mass is not ruptured, below 4 cm, if the HCG level is below 10000 and there is no fetal heartbeat, if the woman’s hemodynamic status is stable and liver-kidney functions are normal, a single dose of methotrexate is applied. Methotrexate treatment is described as the best alternative to surgical treatment.
Methotrexate is basically a drug used in cancer treatment. However, single dose and low dose are applied in the medical treatment of ectopic pregnancy and no serious side effects are expected. The treatment cost is low and it is a suitable choice for the tubes to be recovered with minimal damage. The basic condition of the follow-up is the patient being closely monitored and being conscious.
Surgical Treatment
In cases with surgical indication, if there is no excessive adhesion in the abdomen and intra-abdominal bleeding is not excessive, if the patient is hemodynamically stable, preference should always be laparoscopy.
Two different surgical ways can be chosen in laparoscopy:
1) Linear salphingostomy: The surface of the tube, which is an ectopic pregnancy, is opened in a thin line and the ectopic product is removed and bleeding control is performed. In salphingostomy, fertility is tried to be preserved, but the probability of healthy pregnancy is about 70% afterwards and the possibility of having an ectopic pregnancy again from the same tube has increased.
2) If the woman has completed her fertility, or if the tube is too damaged to protect, or if she has had an ectopic pregnancy for the second time, or if bleeding cannot be controlled, salpingectomy (removal of the tube) can be performed. If the other tube is healthy, it means that fertility continues.
The continuation of fertility is related to the cause of ectopic pregnancy rather than whether or not the tube is removed.






 Turkish
Turkish Deutsch
Deutsch Bu İçeriği Beğendim
Bu İçeriği Beğendim