Blood Incompatibility (Rh Incompatibility)
If mother blood group Rh negative (-) and father blood group Rh positive (+), there is blood incompatibility during pregnancy. Baby blood group is the determining factor in the probability of the problem. If the baby is Rh negative, there will be no problem. However, if the baby is Rh positive, there may be a problem. Problems that can be detected with Rh positive baby are called “Rh isoimmunization”, but not every Rh positive baby perceives problem in blood incompatibility. The Rh antigen is carried in red blood cells called erythrocytes. It is a type of lipoprotein carried on the erythrocyte membrane.
In couples with Rh incompatibility, if the baby is Rh positive, baby blood cells can be transferred to the mother during pregnancy or delivery. In this case, since the mother is Rh negative, she will perceive the Rh antigens completely foreign and develop the antibodies identified as anti-D. This situation rarely causes problems in the current pregnancy. In general, if the baby is again Rh positive, the mother’s immune system remembers the antigen and produces antigens. Since this condition targets the erythrocytes (red blood cells) carrying the Rh antigen on, red blood cells will be tried to be destroyed and the baby will have varying degrees of anemia (anemia). Tissue hypoxia (lack of oxygen) and acidosis occur due to anemia in the baby, which translates into an effort to produce more blood, both in the bone marrow, and in the spleen and liver, and the spleen and liver are growing. After a while, due to the hyperdynamic cycle, heart loading symptoms show and cardiomegaly (heart enlargement) occurs. This severe anemia and heart failure process, which will also affect the decreased protein production in the liver; fetal acid, hydrothorax, scalp edema, swelling in the placenta develop after fetal hydrops fetalis. During this process, polyhdramnios (excessive increase in amniotic fluid) can be seen with increasing urination rate in the baby. Blood flow from the uterus to the placenta may also decrease after some time after the swelling of the placenta called placentomegaly.
The Rh antigen is carried on the short arm of the 1st chromosome. Fetal Rh antigens can be detected on the 30th day after fertilization. Therefore, the baby’s erythrocytes can cause alloimmunization in the mother after 6 weeks of pregnancy.
3 basic conditions are required for Rh alloimunization
1) Mother should be Rh negative and fetus Rh positive
2) Fetal Rh positive erythrocyte should pass into mother’s blood in an amount sufficient to generate sufficient immune response.
3) Must be able to give sufficient immune response to erythrocytes carrying mother D antigen, ie Rh positive antigen.
General approach to Rh incompatibility
First of all, when the woman first applies at the earliest week of pregnancy, the blood group should be determined. If the prospective mother is Rh negative and the prospective father is Rh positive, the woman is monitored monthly with the indirect coombs test. In the indirect coombs test, the amount of antibodies formed against baby erythrocytes in maternal blood can be determined as titration. Patients with negative indirect coombs test are followed up until the 28th week and antenatal prophylaxis (prenatal protection) is performed with 300mg anti-D at 28th week. If the woman gave birth to an Rh positive baby after delivery, 300 mg of anti-D is administered again within the first 72 hours. Although the first 72 hours are important, 14-28 after birth. It is also stated that it can be done until the day. With this precaution, antibody formation will be prevented in the mother, thus avoiding the possibility of problems in the next pregnancy. It is extremely rare to have problems in the first pregnancy in Rh incompatibility. If the baby is Rh negative, anti-D is not applied to the mother. It is never possible to apply anti-D to the baby.
Causes of Rh alloimmunization in pregnancy
- First trimester low
- Ectopic pregnancy
- First trimester miscarriage threat
- Mole pregnancy pregnancy termination in the first and second trimesters
- Fetus death over 10 weeks
- Amniocentesis
- cordocentesis
- Korion vilus biopsy
- Placental detachment (bleeding behind the placenta)
- Abdominal trauma
- In the 2nd and 3rd trimester, the vaginal bleeding with unknown cause
In these cases, it will be appropriate to give the mother 300 mg of anti-D intramuscularly in the first 72 hours. 14-28. It is stated that it can be done until days.
The bleeding rate from fetus to mother was found to be <0.1 in the first trimester abortions. It is known that the amount of blood required for Rh alloimmunization is 0.1 ml. However, the application of anti D seems safe.
There is no point in applying anti-D after the indirect coombs test is positive and should not be done. However, in cases where the blood flow from the fetus to the mother is new and very intense, the mother’s blood, which is normally Rh negative, can be determined as Rh positive. In this case, anti-D should be done.
If indirect coombs are positive, anti D requirement is eliminated and titration is checked. If the titration value is 1/16 and below, there is no significant risk for the fetus in the womb and titration is followed at 2-4 week intervals. No application is required unless the indirect coombs positivity exceeds 1/16. However, if it exceeds 1/16, then detailed ultrasonography, amniocentesis and cordocentesis should be performed in order to understand the size of the process. Hemoglobin measurement and fetal acidosis evaluation can be done with cordocentesis in order to determine the rate of effectiveness of the fetus from the process. If the treatment decision is made, blood transfusion can be done to the baby by cordocentesis. Blood transfusion can be repeated according to the severity of the problem. The rate of pregnancy loss with cordocentesis varies between 0.5% and 2%. Therefore, during cordocentesis to evaluate fetal hemoglobin, blood transfusion should be performed simultaneously to the fetus if deemed necessary. Generally, the place where the umbilical cord (umbilical cord) enters the placenta is preferred. Although intravenous route is preferred for transfusion, pregnancy, intraperitoneal (intraabdominal) transfusion can also be performed in babies with anemia but whose hydrops findings have not yet developed. Both applications can be combined. Transfusion should be repeated every 2-3 weeks. In hydropic infants, transfusion through the vascular access is with higher life percentages. As a result of several transfusion applications, the hydrops findings in the fetus recover rapidly. The plasentomegaly improves at the last attempt.
Transfusion complications; cardiac tamponade, loss of fetus, infection, premature birth and bleeding into amniotic fluid.
Birth time can be determined according to the rate of exposure of fetuses with developed Rh alloimmunization. While mild cases can be expected up to 37-38 weeks with doppler ultrasonography and tight follow-up with NST, the risks of recurrent cordocentesis can be calculated earlier in the heavily affected fetus group, and the decision to give birth can be made earlier. Here, a profit-loss calculation will be made and a decision specific to that pregnancy will be made. In order to accelerate the fetal lung maturation in pregnancies with a premature birth decision, cortisone application to the mother may be considered.
ABO incompatibility
ABO incompatibility is seen in 20% of all pregnancies. Here, the candidate 0 group is the mother. The antibodies develop against the erythrocytes of the baby, which is the A1 and B group. Severe anemia (anemia) is not common in the fetus and the anemia is in mild form.
The most important clinical finding is the bilirubin increase and jaundice, which started in the first 24 hours. Anemia and kernicterus (accumulation of bilirubin in the brain); Unlike Rh incompatibility, it is rare.
In the treatment of ABO incompatibility, 10% probability phototherapy is required to decrease the elevated bilirubin values. Less likely, there could be the cases that require exchange transfusion.






 Turkish
Turkish Deutsch
Deutsch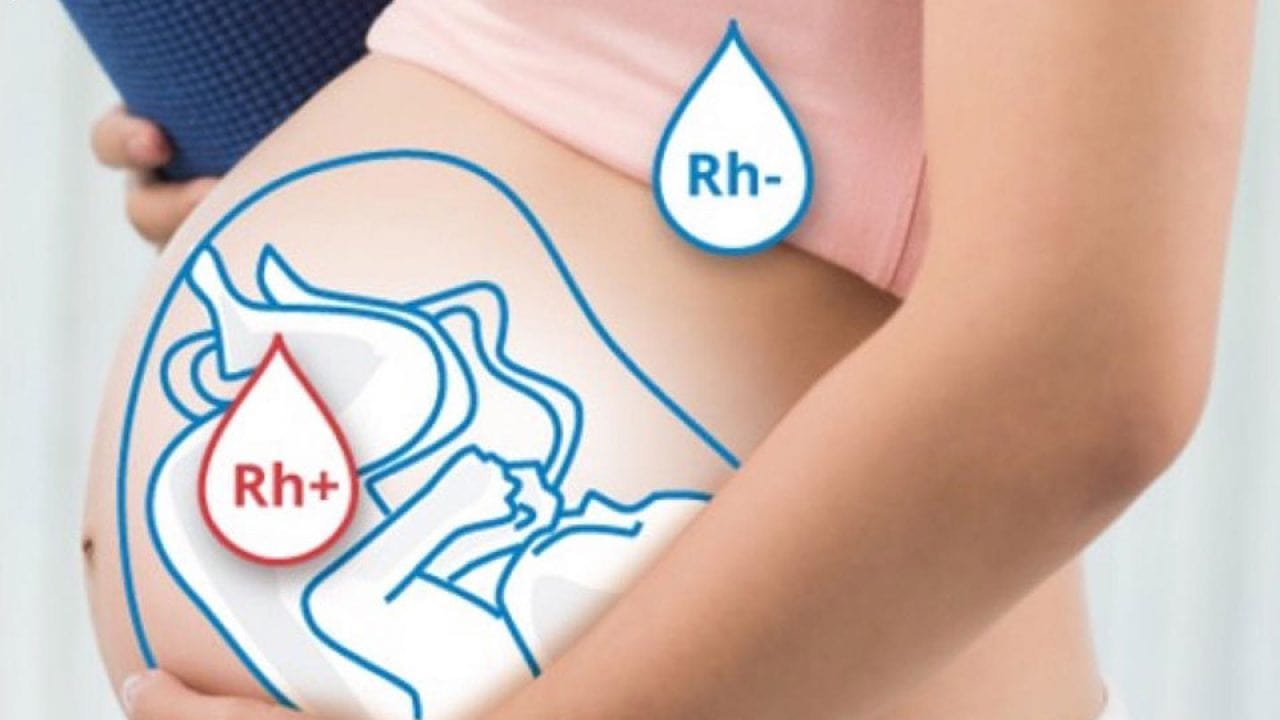
 Bu İçeriği Beğendim
Bu İçeriği Beğendim