Ovary Cancer
Ovarian cancers are the most common cancers in the gynecological cancer ranking in women after uterine cancer.
90% of ovarian cancers are epithelial cancers of the ovary. Cancers of the surface epithelium that cover the ovarian surface and continue with the abdominal membrane. Epithelial ovarian cancers are more common after the age of 55-60, that is, after menopause, but it can also occur in younger women. The remaining 10% of ovarian cancers are caused by non-epithelial cells. These are germ cell tumours (egg cell precursors), sex cord stromal tumours (hormone releasing cells of the ovary), other rare tumours and cancers caused by metastases from other organs. Germ cell tumours constitute 5% of ovarian cancers and are generally found under the age of 30. Sex cord stromal tumours also constitute 5% of ovarian cancers.
Complaints
The most important reason why ovarian cancers cannot be caught early is that they do not usually cause complaints in the early period. Most of the complaints caused by him are of a character that cannot be taken seriously by patients rather than early period. It is the most important step in early diagnosis to evaluate the symptoms at the right time and to consult a specialist and to have regular gynecological controls.
The most common complaints are:
Abdominal pain and groin pain
Abdominal distention, increased abdominal circumference
Feeling of fullness and pressure in the abdomen
Gas, indigestion, nausea
Constipation and diarrhoea attacks
Loss of appetite, quick satiety and weight loss
Low back and back pain
Weakness and fatigue
Screening Methods
A common, easy and inexpensive screening method such as cervical cancer screening with PAP smear is not yet available for ovarian cancers. Still the best method is to evaluate the ovaries in detail with vaginal ultrasonography. It is not suitable to be used as a screening method since tumour markers, which are widely known among the people, can rise in many different situations, especially ca 12-5. However, it would be appropriate to evaluate suspicious cysts or masses or to be used in post-ovarian cancer follow-up.
Assessments Performed for Diagnosis
Cysts or masses present in the ovaries are determined in the gynecological examination performed after the complaints are listened and perceived thoroughly. Afterwards, blood tests called tumour markers and expected to be released from abnormal cells are requested. The most frequently used of these tests in the ovaries are CA 12-5, CA 19-9, ca 15-3 CEA, AFP, HCG and HE4. Since tumour markers can be elevated in many other benign or malignant conditions, the patient’s age, complaints, physical condition, examination findings and ultrasonographic features should be evaluated. HE4 is a tumour marker that has been evaluated with different scoring rates before and after menopause in recent years and may be more specific than CA 12-5.
After the ultrasonography, the pelvic area where the ovaries are located and all the abdominal ultrasonography, magnetic resonance (MR) or computed tomography (CT) or PET can be performed where the organs and lymph nodes in the upper abdomen can be evaluated. Thus, the size of the cyst or kit, its relationship with the surrounding organs, the condition of the bladder and intestines, the condition of the lymph nodes and distant organ metastases can be evaluated. The detailed evaluation made before the treatment begins is very important in the treatment planning.
Protection
The vast majority of ovarian cancers, such as 85%, are epithelial cancers. We now know that epithelial cancers that concern the ovarian surface cell begin at the end of the tubes (fallopian tubes) and then are sown on the ovarian surface. From this point of view, if the woman has completed her fertility and wants her tubes to be connected, it is much more accurate to share this detail with the patient and take the tubes. In cases where the risk of ovarian cancer is high, the preventive measure should be to protect the ovarian tissue and remove the tubes and reduce the risk of ovarian cancer by 85%.
Treatment
Treatment of ovarian cancers is based on surgery. Ovaries, appendages, pelvic and paraaortic lymph nodes are taken, as well as the removal of the ovaries, tubes, and uterus. In the meantime, if tumours are seen at any point in the abdomen, they should be removed. The main goal in surgical treatment is to reduce tumour burden. Survival will be much better if there is no focus in the abdomen and pelvis, or if the remaining tumour tissue is below 1 cm.
If necessary, chemotherapy is applied after surgical treatment.
If there is a relapse in less than 6 months after surgery and chemotherapy, another chemotherapy protocol is applied. If relapse occurred 6 months after the end of chemotherapy, surgery is performed again as much as possible and the mass is cleaned and then chemotherapy is applied again. Recurrence is common in ovarian cancers, so patients should be aware of follow-up
If the woman is young and has not yet had a child, fertility-sparing surgery can be performed if conditions permit. It is legally possible to freeze eggs in our country and can be stored for a long time in a healthy way. However, the effect of choosing fertility-sparing surgery or treatment on the woman’s survival should be thoroughly considered and discussed.
Surgical and oncological treatment of ovarian cancers is a multidisciplinary job. Gynecologist should be applied in a program that oncologists and medical oncologists will conduct with good communication and meticulousness, and the patient should always be operated on specialist hands trained on gynecological oncology.






 Turkish
Turkish Deutsch
Deutsch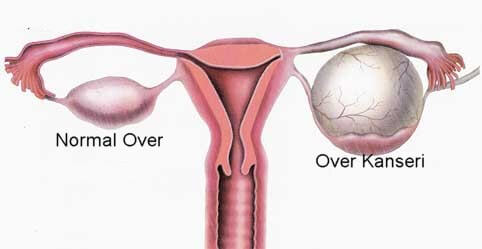
 Bu İçeriği Beğendim
Bu İçeriği Beğendim