Polycystic Ovary Syndrome
Polycystic Ovary Syndrome is observed in 6-8% of the normal population. Monitoring of 10-15 tiny follicles between 2-8 mm in ovaries (ovaries) as a pearl necklace on ultrasonography is called polycystic ovary. If it is monitored only by ultrasonography and without complaints and without clinical findings, it is only called polycystic ovary, which is much more frequent. In the presence of three conditions, called Rotterdam Criteria, we can mention the diagnosis of polycystic ovary syndrome:
1) Ovaries appear polycystic in ultrasonography
2) Inability to see infrequently or without medication due to ovulation difficulties
3) Hyperandrogenemia (hairiness and acne)
While there is a total of 6-7 million follicles in the ovaries of a baby girl in the womb, this number decreases to 2 million at birth. The first girl has approximately 700,000 follicles. With reproductive (productive) life, that is, ovulation from the first menstrual period, the number of follicles gradually decreases.
For many years (up to the age of 18), after the first menstruation of the girl, regular ovulation may not occur and menstrual irregularities may not occur until the harmony between the hypothalamus pituitary axis in the brain and the ovaries occurs. However, if menstrual irregularities persist, there may be several reasons:
1) polycystic ovary syndrome
2) hyperprolactinemia
3) thyroid dysfunctions
4) obesity
5) gaining or losing weight all at once
6) excessive spiritual pressure
7) doing extreme sports, etc.
Among them, the frequency of polycystic ovarian syndrome in young women is quite high and the diagnosis is quite easy.
The Diagnosis of Polycystic Ovary Syndrome
As the diagnostic criteria, we use the criteria set by Rotterdam, ESRE from Europe and ASRM from America, in 2003, which are the two authority groups in the world:
1) the appearance of polycystic ovary in ultrasonography of ovaries (enlarged ovarian volume and 2 or 9 mm size in both ovaries, 12 or more egg sacs)
2) menstrual irregularities (two days have more than 35 days from the previous one, or less than 10 in a year)
3) the high level of male hormone and symptoms.
Of course, in addition to these criteria, we should also use laboratory tests. However, it should be remembered that not all criteria are met or proven at the same time in every woman with PCOS.
Complaints in Polycystic Ovary Syndrome
The most common complaint is sparse menstruation. In addition to this, we may encounter hairiness, easy weight gain and not having children from time to time. Acne development, brown spots and dandruff scalp can also be found as skin findings.
Diagnosis
Ultrasonography (USG) is very helpful in diagnosis, and the typical USG sign in the polycystic ovary is the small follicular 2-8 m, lined up at the periphery of the ovary, like a pearl necklace.
When we try to understand the disruption in the basic hormone functioning of these women, we can actually grasp the syndrome itself quite well.
Normally GnRH from the hypothalamus and then FSH before the pituitary for follicle development, and then LH to provide ovulation. During this process, estrogen and progesterone are secreted from the ovaries in the first half of the cycle, forming a normal menstrual cycle.
Although the cause of the polycystic ovary is not clear, the basic aspects of its functioning can be understood. The main problem here seems to be insulin resistance. Normally, when blood sugar rises after feeding, insulin is secreted from the pancreas and enables the blood sugar to be used by the cells. The excess glucose that cells can use is also stored in the liver and muscles by insulin. Insulin resistance results in the insulin not being able to bind glucose into the cell, and the level of insulin increases gradually to achieve this. The problem is shaped here that the level of insulin in the blood creates an environment that triggers androgen production in the ovaries and the level of androgen increases. Meanwhile, high insulin increases free androgen by decreasing the level of SHBG in the liver. It would be natural for hairiness and / or acne to come into play as a complaint here. High androgen fat is converted to oestrone, an oestrogen derivative, and FSH is suppressed and LH increases. In laboratory findings, high LH / FSH ratio and androgenic hormone increases develop due to this process. This irregularity disrupts the environment required for the regular development of the follicle in the final and the follicle atrophies before it reaches sufficient development. This process forms the basis of ultrasonography findings together with the gradually undeveloped follicle. When the ovulation process is a function close to the outer edge of the ovary, the unfinished follicles are lined up along the outer surface of the ovary and create a traced ultrasonography image like a pearl necklace. If the ovulation problem is persistent or resistant, the woman may encounter the problem of not having children. In laboratory findings, 20% of women with polycystic ovary syndrome may also have high prolactin levels. Polycystic ovarian syndrome is rare and not necessarily seen in all women. Usually one or two of the findings are in the foreground.
Treatment in Polycystic Ovary Syndrome
When focusing on the solution, it is important to perceive what the woman needs in that process. For women who do not want to have a child and want only menstrual order, oral contraceptives (birth control pills) or progesterone preparations can be helped by women. Meanwhile, regular menstruation is not a health requirement. In my own practice, if the patient never wants other methods for the desire to be protected, or if it is not appropriate, I recommend birth control pills. I don’t think it’s too healthy or right to give birth control pills just to create a menstrual cycle.
To ensure that the follicles never form instead of the undeveloped follicles means reducing the androgen-producing environment. If the woman wants a child, it should be worked towards providing ovulation, which will help her have a child and naturally provide menstrual order. Agents that will provide ovulation are the preparations that will be selected exclusively for women, which should be planned by the physician of the patient.
The key point in the treatment is to explain the insulin resistance mechanism to the woman and try to solve it. At this point, ensuring that the woman perceives the issue of increased peripheral adipose tissue, insulin resistance, decrease in metabolic rate and ovulation disorder is the biggest step in breaking the vicious cycle. In this context, it is very important to create a personalized diet and increase exercise. However, these measures are not temporary and should be brought to a lifestyle. Metformin has an important place in breaking insulin resistance and increasing the use of glucose by cells. Metformin, formerly used only in diabetes, is now an important tool for us to increase metabolic rate. If metformin is used with the ideal nutrition and exercise plan, it is very easy to reach all the goals in treatment. The vicious circle in polycystic ovarian syndrome can be destroyed by hitting very target in this sense.
A part of this treatment plan should be perceived as preventive medicine. Because in overweight women with polycystic ovary syndrome, there is an increased risk of endometrial hyperplasia and endometrial cancer due to the transition from advanced insulin resistance to diabetes or exposure to high estrogen and low progesterone levels. Due to obesity and increased androgen levels, hyperlipidaemia and hyper cholesterolemia may be added and the risk of cardiovascular diseases may increase.






 Turkish
Turkish Deutsch
Deutsch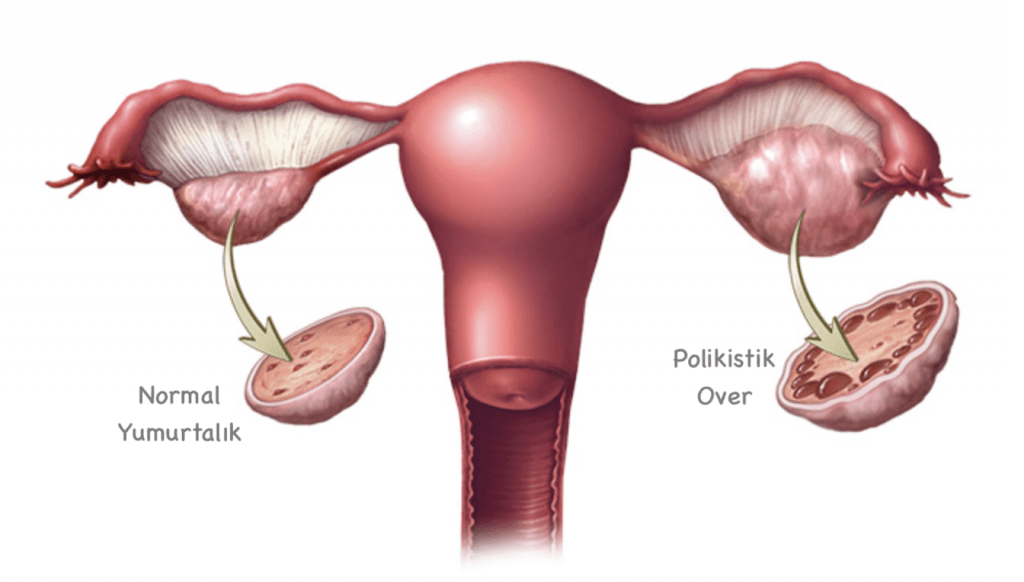
 Bu İçeriği Beğendim
Bu İçeriği Beğendim